Other
(7) Socioeconomic and Demographic Predictors of Transarterial Chemoembolization Outcomes for Hepatic Malignancies
Saturday, September 23, 2023
6:00 PM - 7:30 PM East Coast USA Time
Aaron Chafitz, MD - Ohio State College of Medicine; Rohan Makhijani, BS – Medical Student, Ohio State College of Medicine; Erin Niederkohr, BS – Medical Student, Ohio State College of Medicine; Ian Tarnovksy, BS – Medical Student, Ohio State College of Medicine; Noah Takacs, BS – Medical Student, Ohio State College of Medicine; Xueliang Pan, PhD – Associate Professor, Biomedical Informatics, The Ohio State University; Mina Makary, MD – Clinical Assistant Professor, Division of Vascular and Interventional Radiology, Ohio State Wexner Medical Center
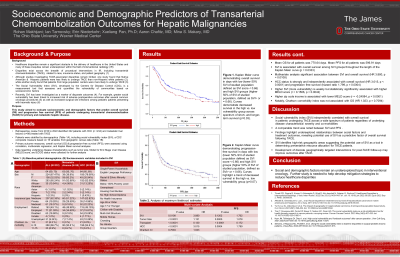
Purpose: This study aimed to evaluate socioeconomic and demographic factors that predict overall survival (OS) and progression free survival (PFS) of patients undergoing transarterial chemoembolization (TACE) for primary and metastatic hepatic disease.
Material and Methods: Retrospective review from 2016 to 2022 identified 322 patients with hepatocellular carcinoma (HCC) (n =234) and metastatic liver lesions (n=98) treated with TACE. Patients were stratified by demographic factors, including average income by zip code, insurance status, race, and social vulnerability index (SVI), a Center for Disease control (CDC) composite measure based on 16 variables from geographic census data. Data regarding underlying disease characteristics such as tumor type, Model for End Stage Liver Disease (MELD) score, Charlson Comorbidity Index, and ECOG performance status. Primary outcomes measures included OS and PFS. Correlation, multivariate regression, and Kaplan Meier survival analyses were performed.
Results: Mean age was 64 years, with 67% were male, 85% were caucasian, and 62% having Medicare coverage. Mean OS was 25.6 months, and PFS was 19.9 months. The disease progression and overall mortality rate were 71.7% and 56.9%, respectively. Lower SVI group, indicating less social vulnerability, was positively associated with OS (p=0.03), and a similar trend was observed for PFS (p=0.07). Co-variate analysis demonstrated statistically significant relationship between SVI and OS (HR=3.880, p=0.01), controlling for underlying disease (HCC vs. mets) and baseline health characteristics. Higher SVI was correlated with higher MELD score (r= 0.16, p < 0.01), and higher zip code income was associated with lower MELD score (r=-0.24, p< 0.01).
Conclusions: Findings highlight underexplored relationships between social factors and treatment outcomes, revealing SVI as a predictive factor of OS following TACE. Further work is needed to better understand disparities associated with procedural interventions in order to target mitigation strategies.
Material and Methods: Retrospective review from 2016 to 2022 identified 322 patients with hepatocellular carcinoma (HCC) (n =234) and metastatic liver lesions (n=98) treated with TACE. Patients were stratified by demographic factors, including average income by zip code, insurance status, race, and social vulnerability index (SVI), a Center for Disease control (CDC) composite measure based on 16 variables from geographic census data. Data regarding underlying disease characteristics such as tumor type, Model for End Stage Liver Disease (MELD) score, Charlson Comorbidity Index, and ECOG performance status. Primary outcomes measures included OS and PFS. Correlation, multivariate regression, and Kaplan Meier survival analyses were performed.
Results: Mean age was 64 years, with 67% were male, 85% were caucasian, and 62% having Medicare coverage. Mean OS was 25.6 months, and PFS was 19.9 months. The disease progression and overall mortality rate were 71.7% and 56.9%, respectively. Lower SVI group, indicating less social vulnerability, was positively associated with OS (p=0.03), and a similar trend was observed for PFS (p=0.07). Co-variate analysis demonstrated statistically significant relationship between SVI and OS (HR=3.880, p=0.01), controlling for underlying disease (HCC vs. mets) and baseline health characteristics. Higher SVI was correlated with higher MELD score (r= 0.16, p < 0.01), and higher zip code income was associated with lower MELD score (r=-0.24, p< 0.01).
Conclusions: Findings highlight underexplored relationships between social factors and treatment outcomes, revealing SVI as a predictive factor of OS following TACE. Further work is needed to better understand disparities associated with procedural interventions in order to target mitigation strategies.
