Musculoskeletal Interventions
(30) Palliative Ablation and Kyphoplasty for a Suspected Metastatic Fracture
Saturday, September 23, 2023
6:00 PM - 7:30 PM East Coast USA Time
Vishal Somnay, MD – Radiology Resident, Radiology, University of Louisville; Henderson Jones, MDJD – Radiology Resident, Radiology, University of Louisville; Nana Ohene Baah, MD – Interventional Radiology Attending, Radiology, University of Louisville
Purpose: We describe the successful radiofrequency ablation (RFA) and subsequent balloon kyphoplasty (BKP) of a painful lytic lesion of the L4 vertebral body in a patient with metastatic renal cell carcinoma. Stereotactic radiosurgery (SRS), first used in the 1950s, provides excellent pain relief but increases vertebral fracture risk. RFA is a relatively new palliative therapy for bony metastases.
Material and Methods: A 61-year-old female with a history of renal cell carcinoma presented with severe lower back pain attributed to a metastatic lesion of L4 with possible vertebral compression fracture. At the time of initial diagnosis 2 years prior, bone scintigraphy demonstrated regions of increased uptake throughout the spine, sacrum, and femurs corresponding to metastatic lesions. The patient elected for ablation and kyphoplasty as opposed to stereotactic radiosurgery.
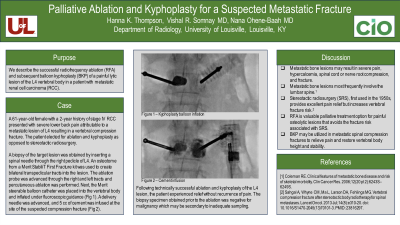
A biopsy of the target lesion was first obtained by inserting a spinal needle through the right L4 pedicle. A Merit StabiliT First Fracture kit was utilized. An osteotome was used to create bilateral transpedicular tracts into the lesion. The ablation probe was advanced through the right and left tracts, and percutaneous ablation was performed. Next, the Merit steerable balloon catheter was placed into the vertebral body and fully inflated under fluoroscopic guidance. A delivery needle was advanced, and 5 cc of cement was infused at the site of the suspected compression fracture.
Results: Following technically successful ablation and kyphoplasty of the L4 lesion, the patient experienced relief without recurrence of pain. The biopsy specimen obtained prior to the ablation was negative for malignancy which may be secondary to inadequate sampling. We maintain a high suspicion that the fracture was indeed pathologic given the positive bone scan.
Conclusions: RFA is a valuable palliative treatment option for painful osteolytic lesions that avoids the fracture risk associated with SRS. BKP may be utilized in metastatic spinal compression fractures to relieve pain and restore vertebral body height and stability.
Material and Methods: A 61-year-old female with a history of renal cell carcinoma presented with severe lower back pain attributed to a metastatic lesion of L4 with possible vertebral compression fracture. At the time of initial diagnosis 2 years prior, bone scintigraphy demonstrated regions of increased uptake throughout the spine, sacrum, and femurs corresponding to metastatic lesions. The patient elected for ablation and kyphoplasty as opposed to stereotactic radiosurgery.
A biopsy of the target lesion was first obtained by inserting a spinal needle through the right L4 pedicle. A Merit StabiliT First Fracture kit was utilized. An osteotome was used to create bilateral transpedicular tracts into the lesion. The ablation probe was advanced through the right and left tracts, and percutaneous ablation was performed. Next, the Merit steerable balloon catheter was placed into the vertebral body and fully inflated under fluoroscopic guidance. A delivery needle was advanced, and 5 cc of cement was infused at the site of the suspected compression fracture.
Results: Following technically successful ablation and kyphoplasty of the L4 lesion, the patient experienced relief without recurrence of pain. The biopsy specimen obtained prior to the ablation was negative for malignancy which may be secondary to inadequate sampling. We maintain a high suspicion that the fracture was indeed pathologic given the positive bone scan.
Conclusions: RFA is a valuable palliative treatment option for painful osteolytic lesions that avoids the fracture risk associated with SRS. BKP may be utilized in metastatic spinal compression fractures to relieve pain and restore vertebral body height and stability.
