Musculoskeletal Interventions
(14) Not novel, but effective! Sclerotherapy for Aneurysmal Bone Cyst
Saturday, September 23, 2023
6:00 PM - 7:30 PM East Coast USA Time
Chadi Diab, MD – Assistant Professor of Radiology, Surgery & Pediatrics, University of Kentucky College of Medicine; Merve Ozen, MD – Assistant Professor of Radiology, Surgery & Pediatrics, University of Kentucky College of Medicine; Driss Raissi, MD – Assistant Professor of Radiology, Surgery & Pediatrics, University of Kentucky College of Medicine; Andrew Shabila, MD – Assistant Professor of Radiology, Surgery & Pediatrics, University of Kentucky College of Medicine; Roberto Galuppo Monticelli, MD – Assistant Professor of Radiology, Surgery & Pediatrics, Radiology and Interventional Radiology, University of Kentucky College of Medicine
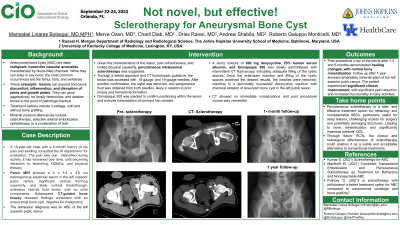
Purpose: A 16-year-old male with a history of hip pain consulted the IR service for evaluation. He described a dull pain
that started 6 months ago and intensifies during activity. It has worsened over time, becoming refractory to
icing, stretching, NSAIDs, and physical therapy. Pelvic MRI showed a 4 x 3.3 x 3.6 cm heterogenous expansile
lesion in the left superior pubic ramus. There was significant cortical thinning superiorly, and likely cortical
breakthrough, extensive internal fluid levels, with no solid components. A subsequent CT-guided bone biopsy
revealed findings consistent with an aneurysmal bone cyst, negative for malignancy.
Material and Methods: His diagnosis upon admission was an aneurysmal bone cyst of the left superior pubic ramus. Given the characteristics of the lesion, pain refractoriness, and limited physical capability, intralesional sclerotherapy is suggested, after discussion of risks and benefits and obtention of informed consent. The procedure was planned as the preferred treatment.
Results: Using a lateral approach and CT fluoroscopic guidance, the aneurysmal bone cyst was accessed with an 18-gauge needle and a 19-gauge needle. After position confirmation, the stylet was removed, and sanguineous fluid was obtained from both needles, likely in relation to prior biopsy and hematoma formation. Omnipaque 300 was injected to confirm positioning within the lesion and exclude intravasation of contrast into vessels. A slurry mixture of 200 mg doxycycline, 25% human serum albumin, and Omnipaque 300 was slowly administered with intermittent CT fluoroscopy, indicating adequate filling of the cystic spaces. Once the sclerosant injection and filling of the cystic spaces achieved the desired results, the needles were removed, resulting in a technically successful doxycycline injection with chemical ablation of aneurysm bone cyst in the
left public lesion. CT showed no immediate complications and post procedural course was uneventful.
Conclusions: Follow-up at 1,3 and 6 months after the procedure, X-ray of the pelvis demonstrated healing changes, with normal bony mineralization. The patient experienced significant clinical improvement, with a remarked reduction in pain and increased functionality in daily activities.
that started 6 months ago and intensifies during activity. It has worsened over time, becoming refractory to
icing, stretching, NSAIDs, and physical therapy. Pelvic MRI showed a 4 x 3.3 x 3.6 cm heterogenous expansile
lesion in the left superior pubic ramus. There was significant cortical thinning superiorly, and likely cortical
breakthrough, extensive internal fluid levels, with no solid components. A subsequent CT-guided bone biopsy
revealed findings consistent with an aneurysmal bone cyst, negative for malignancy.
Material and Methods: His diagnosis upon admission was an aneurysmal bone cyst of the left superior pubic ramus. Given the characteristics of the lesion, pain refractoriness, and limited physical capability, intralesional sclerotherapy is suggested, after discussion of risks and benefits and obtention of informed consent. The procedure was planned as the preferred treatment.
Results: Using a lateral approach and CT fluoroscopic guidance, the aneurysmal bone cyst was accessed with an 18-gauge needle and a 19-gauge needle. After position confirmation, the stylet was removed, and sanguineous fluid was obtained from both needles, likely in relation to prior biopsy and hematoma formation. Omnipaque 300 was injected to confirm positioning within the lesion and exclude intravasation of contrast into vessels. A slurry mixture of 200 mg doxycycline, 25% human serum albumin, and Omnipaque 300 was slowly administered with intermittent CT fluoroscopy, indicating adequate filling of the cystic spaces. Once the sclerosant injection and filling of the cystic spaces achieved the desired results, the needles were removed, resulting in a technically successful doxycycline injection with chemical ablation of aneurysm bone cyst in the
left public lesion. CT showed no immediate complications and post procedural course was uneventful.
Conclusions: Follow-up at 1,3 and 6 months after the procedure, X-ray of the pelvis demonstrated healing changes, with normal bony mineralization. The patient experienced significant clinical improvement, with a remarked reduction in pain and increased functionality in daily activities.
