Hepatocellular Carcinoma
(28) Rapid extra segmental metastases of Hepatocellular Carcinoma following Transarterial Chemoembolization: Two Cases
Saturday, September 23, 2023
6:00 PM - 7:30 PM East Coast USA Time
Aishwarya Thakurdesai, MD – Resident Physician, Internal Medicine, University of Louisville Hospitals; Michael Shumaker, MD – Resident Physician, Radiology, University of Louisville Hospitals; Ashutosh Barve, MD – Professor, Gastroenterology, University of Louisville Hospitals; Sohail Contractor, MD – Professor and Chair, Radiology, University of Louisville Hospitals
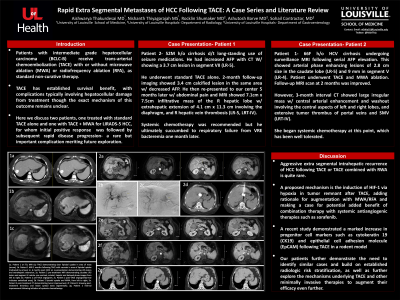
Purpose: Patients with intermediate grade hepatocellular carcinoma (HCC; BCLC-B) receive trans-arterial chemoembolization (TACE) as standard therapy. TACE has established survival benefit, with complications typically involving hepatocellular damage from treatment. A rare but important complication of TACE is rapid development of new intrahepatic HCC following an initial positive response to TACE on interval imaging. Here we discuss two patients, one treated with standard TACE alone and one with TACE + MWA for LIRADS-5 HCC, for whom initial positive response was followed by subsequent rapid disease progression.
Material and Methods: Patient 1- 66F h/o HCV cirrhosis undergoing surveillance MRI following serial AFP elevation. This showed arterial phase enhancing lesions of 2.8 cm size in the caudate lobe (LR-5) and 9 mm in segment V (LR-4). Patient underwent TACE and MWA ablation. Follow-up MRI scan at 2 months was improved. However, 3-month interval CT showed large irregular mass w/ central arterial enhancement and washout involving the central aspects of left and right lobes, and extensive tumor thrombus of portal veins and SMV (LRT-IV). She began systemic chemotherapy at this point, which has been well tolerated.
Results: Patient 2- 52M h/o cirrhosis d/t long-standing use of seizure medications. He had increased AFP with CT W/ showing a 3.7 cm lesion in segment VII (LR-5). He underwent standard TACE alone. 2-month follow-up imaging showed 3.4 cm calcified lesion in the same area w/ decreased AFP. He then re-presented to our center 5 months later w/ abdominal pain and MRI showed 7.1cm x 7.5cm infiltrative mass of the R hepatic lobe w/ extrahepatic extension of 4.1 cm x 11.3 cm involving the diaphragm, and R hepatic vein thrombosis (LR-5, LRT-IV). Systemic chemotherapy was recommended but he ultimately succumbed to respiratory failure from VRE bacteremia one month later.
Conclusions: Aggressive extra segmental intrahepatic recurrence of HCC following TACE is quite rare. One proposed mechanism is the induction of HIF-1, explaining potential added benefit of combination therapy with systemic antiangiogenic therapies such as sorafenib. Our patients further demonstrate the need to identify similar patients and build on established radiologic risk stratification, as well as consider alternative embolization strategies in concurrence with medical treatment.
Material and Methods: Patient 1- 66F h/o HCV cirrhosis undergoing surveillance MRI following serial AFP elevation. This showed arterial phase enhancing lesions of 2.8 cm size in the caudate lobe (LR-5) and 9 mm in segment V (LR-4). Patient underwent TACE and MWA ablation. Follow-up MRI scan at 2 months was improved. However, 3-month interval CT showed large irregular mass w/ central arterial enhancement and washout involving the central aspects of left and right lobes, and extensive tumor thrombus of portal veins and SMV (LRT-IV). She began systemic chemotherapy at this point, which has been well tolerated.
Results: Patient 2- 52M h/o cirrhosis d/t long-standing use of seizure medications. He had increased AFP with CT W/ showing a 3.7 cm lesion in segment VII (LR-5). He underwent standard TACE alone. 2-month follow-up imaging showed 3.4 cm calcified lesion in the same area w/ decreased AFP. He then re-presented to our center 5 months later w/ abdominal pain and MRI showed 7.1cm x 7.5cm infiltrative mass of the R hepatic lobe w/ extrahepatic extension of 4.1 cm x 11.3 cm involving the diaphragm, and R hepatic vein thrombosis (LR-5, LRT-IV). Systemic chemotherapy was recommended but he ultimately succumbed to respiratory failure from VRE bacteremia one month later.
Conclusions: Aggressive extra segmental intrahepatic recurrence of HCC following TACE is quite rare. One proposed mechanism is the induction of HIF-1, explaining potential added benefit of combination therapy with systemic antiangiogenic therapies such as sorafenib. Our patients further demonstrate the need to identify similar patients and build on established radiologic risk stratification, as well as consider alternative embolization strategies in concurrence with medical treatment.
