Ablative Therapy
(18) Pulsed Electric Field Therapy Enhances Survival in Murine Breast Cancer Models Relative to Thermal Ablation
Saturday, September 23, 2023
6:00 PM - 7:30 PM East Coast USA Time
Chiara Pastori, Ph.D – Associate Director, Oncology department, Galvanize Therapeutics; Ella Goldschmidt, Master – Associate Research Scientist, Oncology department, Galvanize Therapeutics; Mukta Wagh, Master – Associate Research Scientist, Oncology department, Galvanize Therapeutics; Robert Neal, Ph.D – Sr. Director of research, Oncology department, Galvanize Therapeutics
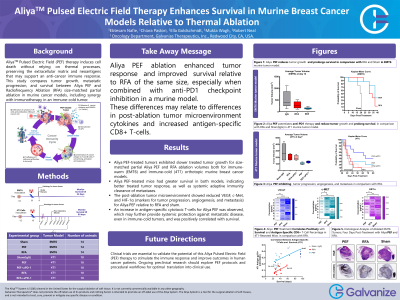
Purpose: Pulsed Electric Field (PEF) therapy induces cell death without thermal processes, preserving extracellular matrix and neoantigens that may support an anti-cancer immune response. This study compares tumor growth, metastatic progression and survival between PEF and radiofrequency ablation (RFA) in murine breast cancer models. The synergistic effect of PEF and immunotherapy is also explored.
Material and Methods: Murine triple-negative breast cancer cell lines (EMT6; 4T1) were used to establish orthotopic breast tumors in female Balb/c mice. Proprietary PEF energy was used to match RFA ablation zones, targeting about 80% tumor volume. Histological analysis confirmed ablation efficacy. A subset of mice received anti-PD-1 immunotherapy. A Sham group underwent a procedure without ablation. Outcomes included survival and cytokine analyses at several time points.
Results: All mice tolerated PEF and RFA well. PEF and RFA demonstrated similar ablation volumes, but PEF-treated tumors exhibited immune infiltration throughout the ablation zone, while RFA-treated tumors showed necrosis and immune cells at treatment margins. PEF-treated tumors (EMT6 and 4T1) exhibited significantly slower growth (p < 0.05) compared to RFA and Sham treatment, despite equivalent treatment volumes. Kaplan-Meier survival (EMT6) at day 45 was 37.5%, 12.5%, and 0% in PEF, RFA, and sham groups, respectively. For 4T1, these values were 20%, 0%, and 0%, respectively, at day 80. Combining PEF with anti-PD-1 antibody improved survival to 40% at day 80 for 4T1. HIF-α levels were significantly decreased by 1.7-fold in PEF group compared to RFA and 1.8-fold compared to Sham (p < 0.001). VEGF levels were significantly decreased by 5.2-fold in PEF group vs. RFA and 7.9-fold compared to Sham (p < 0.001). c-Met expression was significantly lower in the PEF group than RFA and sham (p < 0.05), indicating efficacy in inhibiting tumor progression, angiogenesis, and metastasis.
Conclusions: The PEF treatment evaluated in this murine model was superior to RFA in terms of immune infiltration and tumor response. PEF-treated tumors displayed a robust immune response throughout the ablation zone, which may have contributed to improved survival outcomes. These findings, bolstered by the results of PEF when combined with immune checkpoint inhibitors suggest the potential for PEF as a promising ablation technique for cancer treatment in humans.
Material and Methods: Murine triple-negative breast cancer cell lines (EMT6; 4T1) were used to establish orthotopic breast tumors in female Balb/c mice. Proprietary PEF energy was used to match RFA ablation zones, targeting about 80% tumor volume. Histological analysis confirmed ablation efficacy. A subset of mice received anti-PD-1 immunotherapy. A Sham group underwent a procedure without ablation. Outcomes included survival and cytokine analyses at several time points.
Results: All mice tolerated PEF and RFA well. PEF and RFA demonstrated similar ablation volumes, but PEF-treated tumors exhibited immune infiltration throughout the ablation zone, while RFA-treated tumors showed necrosis and immune cells at treatment margins. PEF-treated tumors (EMT6 and 4T1) exhibited significantly slower growth (p < 0.05) compared to RFA and Sham treatment, despite equivalent treatment volumes. Kaplan-Meier survival (EMT6) at day 45 was 37.5%, 12.5%, and 0% in PEF, RFA, and sham groups, respectively. For 4T1, these values were 20%, 0%, and 0%, respectively, at day 80. Combining PEF with anti-PD-1 antibody improved survival to 40% at day 80 for 4T1. HIF-α levels were significantly decreased by 1.7-fold in PEF group compared to RFA and 1.8-fold compared to Sham (p < 0.001). VEGF levels were significantly decreased by 5.2-fold in PEF group vs. RFA and 7.9-fold compared to Sham (p < 0.001). c-Met expression was significantly lower in the PEF group than RFA and sham (p < 0.05), indicating efficacy in inhibiting tumor progression, angiogenesis, and metastasis.
Conclusions: The PEF treatment evaluated in this murine model was superior to RFA in terms of immune infiltration and tumor response. PEF-treated tumors displayed a robust immune response throughout the ablation zone, which may have contributed to improved survival outcomes. These findings, bolstered by the results of PEF when combined with immune checkpoint inhibitors suggest the potential for PEF as a promising ablation technique for cancer treatment in humans.
