Radioembolization
(34) Radioembolization plus Gemcitabine, Cisplatin and Capecitabine as First-Line Therapy for Intrahepatic Cholangiocarcinoma
Saturday, September 23, 2023
6:00 PM - 7:30 PM East Coast USA Time
Qian Yu, MD; Yating Wang, MD – MD, Ascension Providence Hospital; Mikin Patel, MD – Doctor, University of Chicago; Thuong Van Ha, MD – MD, University of Chicago; John Fung, MD – Professor, University of Chicago; Anjana Pillai, MD – Associate Professor, University of Chicago; Chih-yi Liao, MD – Associate Professor, University of Chicago; Talia Baker, MD – Professor, University of Utah; Osman Ahmed, MD – Associate Professor, University of Chicago
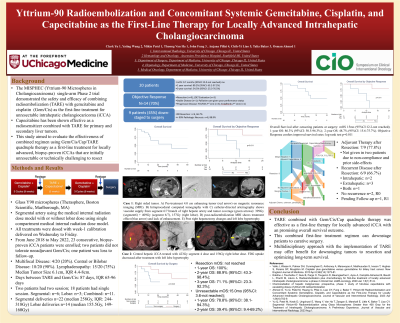
Purpose: To report outcomes of an institutional downstaging protocol for intrahepatic cholangiocarcinoma (iCCA) using radioembolization (TARE), gemcitabine, cisplatin, and capecitabine combination as the first-line therapy.
Material and Methods: From June 2018 to May 2022, 23 consecutive patients with treatment-naïve, locally advanced iCCA were enrolled in an institutional downstaging protocol. Patients received intravenous gemcitabine (1,000 mg/m2) and cisplatin (25 mg/m2) on days 1 and 8 over a 21-day cycle for 3 cycles, followed by oral capecitabine (1,000 mg/m2) twice daily for 14 days in a 21-day cycle for 1 or 2 cycles. TARE was performed with glass microspheres using the medical internal radiation dose model. An additional 3 cycles of gemcitabine and cisplatin were administered, followed by restaging scans and evaluation for resectability. Objective response was assessed with Response Evaluation Criteria in Solid Tumors 1.1 criteria. Overall survival (OS) was assessed with Kaplan-Meier method.
Results: Two patients did not tolerate pre-TARE systemic therapy and transitioned to supportive care. One patient was lost to follow-up after TARE. Objective response was achieved in the remaining 14/20 (70.0%) patients. OS at 1-year, 2-year, and 3-year OS were 84.7% (95%CI: 59.7-94.8%), 62.1% (95%CI: 36.4-79.9%), and 51.8% (95%CI: 24.1-73.7%), respectively, with a median survival time (MST) of 40.7 (95%CI:15.0-not reached) months. Nine patients were downstaged to resection post-TARE (9/21, 42.9%). Three non-resection candidates with objective response were undergoing evaluation for living donor liver transplant given local disease stability. One patient with object response lost surgical candidacy due to malnutrition despite objective response. Patients who were bridged to surgery demonstrated longer MST (not reached versus 13.7 months, p=0.025). Patients who achieved objective response upon completion of downstaging protocol showed longer MST (not reached vs 12.2 months, p< 0.001).
Conclusions: First line therapy using radioembolization, gemcitabine, cisplatin, and capecitabine was effective for locally advanced iCCA in achieving objective response and downstage to surgery.
Material and Methods: From June 2018 to May 2022, 23 consecutive patients with treatment-naïve, locally advanced iCCA were enrolled in an institutional downstaging protocol. Patients received intravenous gemcitabine (1,000 mg/m2) and cisplatin (25 mg/m2) on days 1 and 8 over a 21-day cycle for 3 cycles, followed by oral capecitabine (1,000 mg/m2) twice daily for 14 days in a 21-day cycle for 1 or 2 cycles. TARE was performed with glass microspheres using the medical internal radiation dose model. An additional 3 cycles of gemcitabine and cisplatin were administered, followed by restaging scans and evaluation for resectability. Objective response was assessed with Response Evaluation Criteria in Solid Tumors 1.1 criteria. Overall survival (OS) was assessed with Kaplan-Meier method.
Results: Two patients did not tolerate pre-TARE systemic therapy and transitioned to supportive care. One patient was lost to follow-up after TARE. Objective response was achieved in the remaining 14/20 (70.0%) patients. OS at 1-year, 2-year, and 3-year OS were 84.7% (95%CI: 59.7-94.8%), 62.1% (95%CI: 36.4-79.9%), and 51.8% (95%CI: 24.1-73.7%), respectively, with a median survival time (MST) of 40.7 (95%CI:15.0-not reached) months. Nine patients were downstaged to resection post-TARE (9/21, 42.9%). Three non-resection candidates with objective response were undergoing evaluation for living donor liver transplant given local disease stability. One patient with object response lost surgical candidacy due to malnutrition despite objective response. Patients who were bridged to surgery demonstrated longer MST (not reached versus 13.7 months, p=0.025). Patients who achieved objective response upon completion of downstaging protocol showed longer MST (not reached vs 12.2 months, p< 0.001).
Conclusions: First line therapy using radioembolization, gemcitabine, cisplatin, and capecitabine was effective for locally advanced iCCA in achieving objective response and downstage to surgery.
