(35) Percutaneous Ablation of Colorectal Liver Metastasis in a Patient with Hereditary Hemorrhagic Telangiectasia
Saturday, September 23, 2023
6:00 PM - 7:30 PM East Coast USA Time
Ashwin M Mahendra BS1, Yaell Livni BS2, Govindarajan Narayanan MD2,3
Florida Atlantic University Charles E. Schmidt College of Medicine, Boca Raton FL1
Florida International University Herbert Wertheim College of Medicine, Miami FL2
Miami Cancer Institute, Miami FL3
Florida Atlantic University Charles E. Schmidt College of Medicine, Boca Raton FL1
Florida International University Herbert Wertheim College of Medicine, Miami FL2
Miami Cancer Institute, Miami FL3
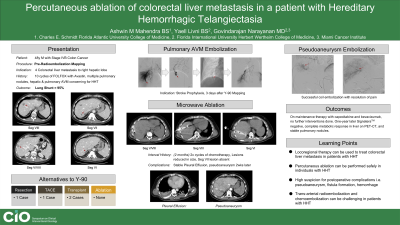
Purpose: Hereditary Hemorrhagic Telangiectasia (HHT) is a rare, autosomal dominant disorder characterized by recurrent epistaxis, telangiectasias, and visceral arteriovenous malformations (AVM). Endovascular, percutaneous, and surgical procedures of the liver are generally avoided in patients with HHT due to high risk of bleeding. We present the case of a patient with HHT and colorectal liver metastasis (CRLM) who was successfully managed with percutaneous microwave ablation.
Material and Methods: To the best of our knowledge, only five studies have described the treatment of hepatic tumors in patients with HHT. All discuss treatment of hepatocellular carcinoma (HCC) with either liver transplantation, surgical resection, or transarterial chemoembolization (TACE). This is the first report describing locoregional therapy of CRLMs and the use of percutaneous ablation in the liver of patients with HHT.
Results: The patient presented for Yittrium-90 (Y90) pre-planning. Prior imaging demonstrated four CRLMs in the right hepatic lobe, stable pulmonary nodules, and two arteriovenous malformations (AVM) concerning for HHT. The patient was found to meet the Curaçao criteria (4/4) for HHT. Preradioembolization planning demonstrated a high lung shunt fraction of 95%, consistent with arteriovenous shunting secondary to HHT. TACE was not advised due to concerns of poor efficacy given the evidence of significant hepatic shunting. Given the multitude of hepatic small lesions (all <3 cm), surgery was thought to carry a high risk of bleeding and percutaneous microwave ablation was advised. The patient underwent successful embolization of the pulmonary AVM to reduce risk of stroke during future hepatic interventions. Two months later microwave ablation with tract ablation was done over three lesions, the fourth previously detected lesion could not be visualized. During the immediate postoperative period, the patient only reported mild abdominal pain. At two-week follow up, the patient continued to report abdominal pain. Imaging showed a 2.6 cm pseudo-aneurysm along one of the ablation tracts. The pseudoaneurysm was successfully coil embolized. The patient has not had any other procedures since. At one-year follow-up, the patient is Signetera™ negative and has achieved a complete metabolic response in all liver lesions on positron-emission tomography (PET). Hepatic lesions are all significantly diminished in size and pulmonary deposits have remained stable in size since induction chemotherapy.
Conclusions: Percutaneous ablation is a safe and effective procedure in the management of CRLM in patients with HHT. These patients are at high-risk of bleeding and operators should approach treatment in these patients with careful planning, a high index of clinical suspicion for vascular complications, and close follow-up.
Material and Methods: To the best of our knowledge, only five studies have described the treatment of hepatic tumors in patients with HHT. All discuss treatment of hepatocellular carcinoma (HCC) with either liver transplantation, surgical resection, or transarterial chemoembolization (TACE). This is the first report describing locoregional therapy of CRLMs and the use of percutaneous ablation in the liver of patients with HHT.
Results: The patient presented for Yittrium-90 (Y90) pre-planning. Prior imaging demonstrated four CRLMs in the right hepatic lobe, stable pulmonary nodules, and two arteriovenous malformations (AVM) concerning for HHT. The patient was found to meet the Curaçao criteria (4/4) for HHT. Preradioembolization planning demonstrated a high lung shunt fraction of 95%, consistent with arteriovenous shunting secondary to HHT. TACE was not advised due to concerns of poor efficacy given the evidence of significant hepatic shunting. Given the multitude of hepatic small lesions (all <3 cm), surgery was thought to carry a high risk of bleeding and percutaneous microwave ablation was advised. The patient underwent successful embolization of the pulmonary AVM to reduce risk of stroke during future hepatic interventions. Two months later microwave ablation with tract ablation was done over three lesions, the fourth previously detected lesion could not be visualized. During the immediate postoperative period, the patient only reported mild abdominal pain. At two-week follow up, the patient continued to report abdominal pain. Imaging showed a 2.6 cm pseudo-aneurysm along one of the ablation tracts. The pseudoaneurysm was successfully coil embolized. The patient has not had any other procedures since. At one-year follow-up, the patient is Signetera™ negative and has achieved a complete metabolic response in all liver lesions on positron-emission tomography (PET). Hepatic lesions are all significantly diminished in size and pulmonary deposits have remained stable in size since induction chemotherapy.
Conclusions: Percutaneous ablation is a safe and effective procedure in the management of CRLM in patients with HHT. These patients are at high-risk of bleeding and operators should approach treatment in these patients with careful planning, a high index of clinical suspicion for vascular complications, and close follow-up.
