Other Organ Systems
(23) Efficacy and Safety of Intraarterial Chemotherapy in Locally Aggressive Breast Cancers: A 10-Year Literature Review
Saturday, September 23, 2023
6:00 PM - 7:30 PM East Coast USA Time
Chris Yeisley, MD – Resident, Interventional Radiology, Northwell Health; Mustafa Al-Roubaie, MD – Assistant Professor, Interventional Radiology, Moffitt Cancer Center
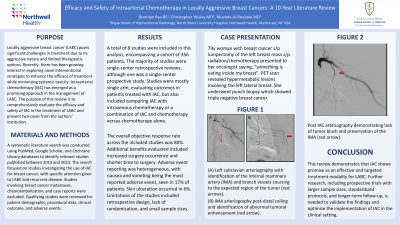
Purpose: Locally aggressive breast cancer (LABC) poses significant challenges in treatment due to its aggressive nature and limited therapeutic options. Recently, there has been growing interest in exploring novel interventional strategies to enhance the efficacy of treatment while minimizing systemic toxicity. Intraarterial chemotherapy (IAC) has emerged as a promising approach in the management of LABC. The purpose of this review is to comprehensively evaluate the efficacy and safety of IAC in the treatment of LABC and present two cases from the authors’ institution.
Material and Methods: A systematic literature search was conducted using PubMed, Google Scholar, and Cochrane Library databases to identify relevant studies published between 2013 and 2023. The search focused on studies investigating the use of IAC for breast cancer, with specific attention given to LABC and recurrent disease. Studies involving breast cancer metastases, chemoembolization, and case reports were excluded. Qualifying studies were reviewed for patient demographic, procedural data, clinical outcome, and adverse events.
Results: A total of 8 studies were included in this analysis, encompassing a cohort of 356 patients. The majority of studies were single-center retrospective reviews, although one was a single-center prospective study. Studies were mostly single arm, evaluating outcomes in patients treated with IAC, but also included comparing IAC with intravenous chemotherapy or a combination of IAC and chemotherapy versus chemotherapy alone.
The overall objective response rate across the included studies was 80%. Additional benefits evaluated included increased surgery occurrence and shorter time to surgery. Adverse event reporting was heterogeneous, with nausea and vomiting being the most reported adverse event, seen in 17% of patients. Skin ulceration occurred in 6%. Limitations of the studies included retrospective design, lack of randomization, and small sample sizes.
Conclusions: This review demonstrates that IAC shows promise as an effective and targeted treatment modality for LABC. Further research, including prospective trials with larger sample sizes, standardized protocols, and longer-term follow-up, is needed to validate the findings and optimize the implementation of IAC in the clinical setting.
Material and Methods: A systematic literature search was conducted using PubMed, Google Scholar, and Cochrane Library databases to identify relevant studies published between 2013 and 2023. The search focused on studies investigating the use of IAC for breast cancer, with specific attention given to LABC and recurrent disease. Studies involving breast cancer metastases, chemoembolization, and case reports were excluded. Qualifying studies were reviewed for patient demographic, procedural data, clinical outcome, and adverse events.
Results: A total of 8 studies were included in this analysis, encompassing a cohort of 356 patients. The majority of studies were single-center retrospective reviews, although one was a single-center prospective study. Studies were mostly single arm, evaluating outcomes in patients treated with IAC, but also included comparing IAC with intravenous chemotherapy or a combination of IAC and chemotherapy versus chemotherapy alone.
The overall objective response rate across the included studies was 80%. Additional benefits evaluated included increased surgery occurrence and shorter time to surgery. Adverse event reporting was heterogeneous, with nausea and vomiting being the most reported adverse event, seen in 17% of patients. Skin ulceration occurred in 6%. Limitations of the studies included retrospective design, lack of randomization, and small sample sizes.
Conclusions: This review demonstrates that IAC shows promise as an effective and targeted treatment modality for LABC. Further research, including prospective trials with larger sample sizes, standardized protocols, and longer-term follow-up, is needed to validate the findings and optimize the implementation of IAC in the clinical setting.
